A $70 million pilot program to deliver malaria vaccines was rolled out in Africa in 2019, and analysis of the initiative has revealed stunning results.
In October, the World Health Organization (WHO) found that a three-dose vaccine caused deaths to drop by 13% in young children over the course of the four-year program, as reported by Science.
"I was surprised I didn't hear any gasps when it was stated," medical epidemiologist Mary Hamel, who led the WHO pilot program, told the outlet of the incredible drop in deaths.
The vaccine, which was made by GlaxoSmithKline, also reduced severe cases of the disease by 22% in children, who are most vulnerable to the infections.
"The data speak for themselves," added physician and epidemiologist Kwaku Poku Asante, the director of Kintampo Health Research Centre and overseer of the analysis in Ghana. "This was a very large, very robust evaluation done in a real-life setting, and you're seeing this huge impact."
Almost two million "very young children" received the vaccine across Ghana, Kenya, and Malawi, according to Science. Researchers also studied whether the vaccine — known as RTS,S, or Mosquirix — could be successfully administered without affecting other life-saving vaccines that children typically receive.
According to the WHO, immunizations already save an estimated 4 to 5 million lives annually, and another 1.5 million deaths could be prevented if access to them is expanded. However, until 2021, as noted by Science, there was no approved vaccine for malaria, which killed almost half a million children in sub-Saharan Africa that same year.
Africa is disproportionately impacted by infections, with the health organization noting that 94% of malaria cases occurred in the WHO's African region, which encompasses 48 of the 54 countries on the continent that are also members of the United Nations.
The disease, which is overwhelmingly spread by infected mosquitoes, is most common in tropical and subtropical climates. Almost half of the worldwide population lives in at-risk regions, and rising global temperatures have raised concerns that new areas will see an increase in the disease, as insects are able to thrive in higher altitudes.
Hamel pointed out to Science that the pilot program may have created "a delay in widespread use of the [malaria] vaccine," but she is hopeful it answered potential questions about its safety and that the data could be used in the development of other malaria vaccines.
Cameroon just launched the first-ever mass vaccination program for malaria with RTS,S in early 2024, and Science notes that 17 total countries in Africa had greenlit their own campaigns as of October 2023. The approval of the R21, or Matrix-M, vaccine for release later this year may lead to even further relief in the near future.
"As a malaria researcher, I used to dream of the day we would have a safe and effective vaccine against malaria. Now we have two," WHO director-general Dr. Tedros Adhanom Ghebreyesus said in a statement for the organization. "Demand for the RTS,S vaccine far exceeds supply, so this second vaccine is a vital additional tool to protect more children faster, and to bring us closer to our vision of a malaria-free future."
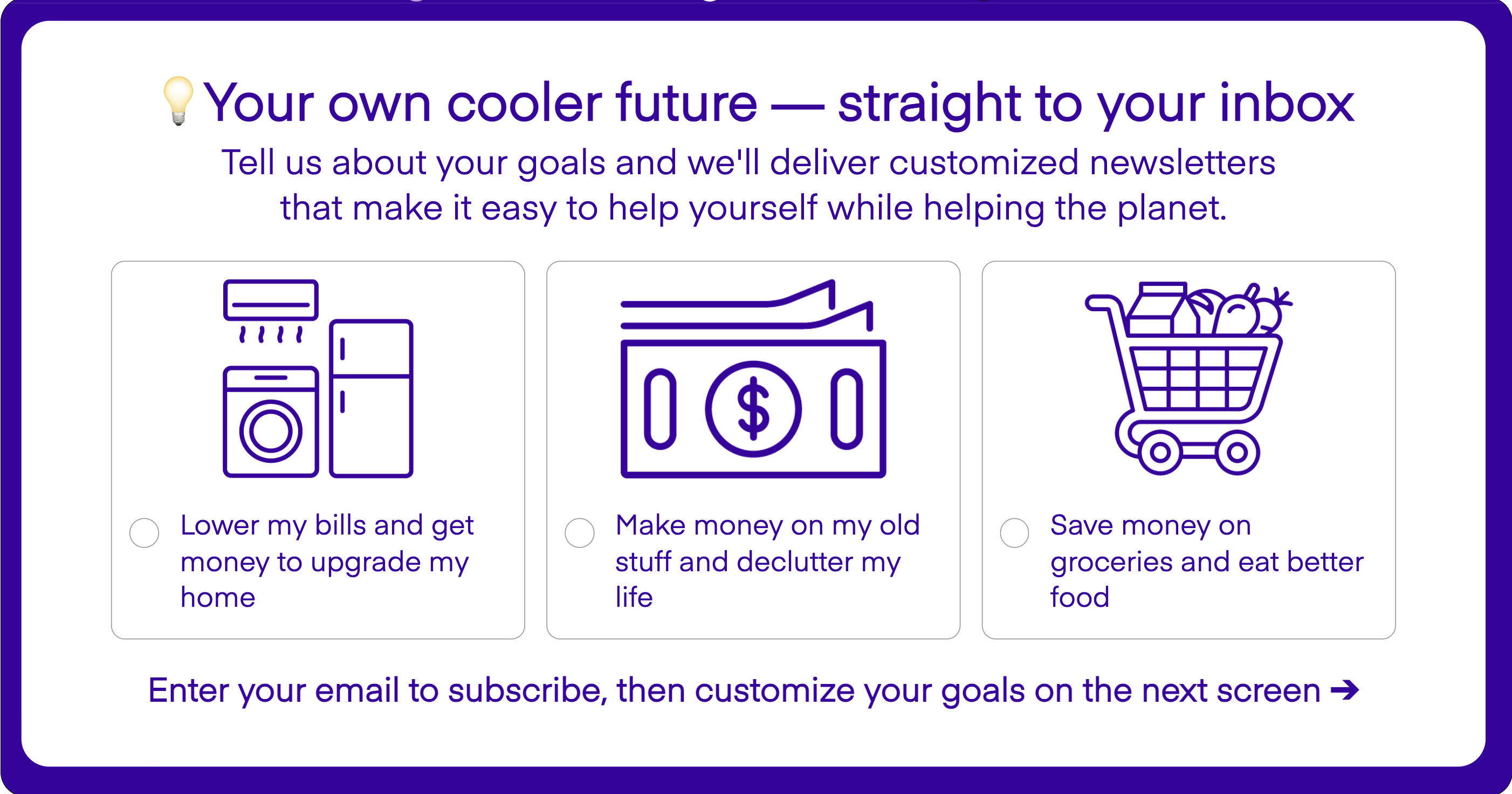
Join our free newsletter for weekly updates on the coolest innovations improving our lives and saving our planet.